Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Oral & Maxillofacial Space Infections – A 10-Year Retrospective Study
*Corresponding author:Ashok Jogpal, Oral and Maxillofacial Surgery, Defence Hospital, India.
Received:March 06, 2023; Published:April 10, 2023
DOI: 10.34297/AJBSR.2023.18.002477
Abstract
Keywords: Maxillofacial infections, Odontogenic infections, Complications, Surgical drainage.
Introduction
Oral & Maxillofacial space infections have been recognized since the time of Galen in the second century. In spite of great advances in health care, these infections remain a major problem. Oral & Maxillofacial space infection ranges from periapical abscess to superficial and deep neck infections. The infections generally follow the path of least resistance through connective tissue and along fascial planes [1]. The infections spread to distant sites from the site of origin. Oral & Maxillofacial infections can be potentially lethal infections, at times [2]. Various life-threatening complications associated with oral & maxillofacial infections are respiratory obstruction, [3] necrotizing fasciitis, [4-8] descending mediastinitis, [5] pericarditis, [5] brain abscess, [4] and sepsis [4]. The successful management of orofacial infection depends on the early recognition of orofacial infection. Appropriate and prompt therapy is mandatory for successful management. Thorough knowledge of anatomy is necessary to predict pathways of spread and to drain these spaces adequately. We present our experience in treating oral & maxillofacial space infection at our centre.
Methods
The patients with oral & maxillofacial surgery infection who reported to our centre from Jan 2012 to Jan 2022 were included in the study. Only patients with any threat to the airway, fever greater than 38 ℃, need for general anaesthesia and need for control of a concomitant systemic disease were admitted. Rest all other patients were treated as outpatients. Haematological and biochemical tests were done on all the admitted patients. Empirical antibiotics orally or through an intravenous route were given as per the indications. In all patient incision and drainage was carried out under LA or GA depending on the patient’s condition. Spaces were decompressed even in the patients in which pus was not formed. A drain was placed in every patient. The causative teeth were extracted. Patient was followed till the complete resolution of infection.
Data Collection
A retrospective medical finding of patients with a diagnosis of oral & maxillofacial surgical space infection was recorded. Clinical charts and investigation reports were reviewed. These variables were recorded systematically: demographic data (age, sex), etiopathogenesis (aetiology, number and location of teeth involved, spaces involved, associated systemic diseases), clinical presentation (presenting symptoms, time from onset of symptoms until presentation, the temperature at presentation), blood sugars, medical treatment (antibiotics used), surgical treatment (type of anaesthesia, intubation, incision, usage of drains), and outcome (complications, duration of stay).
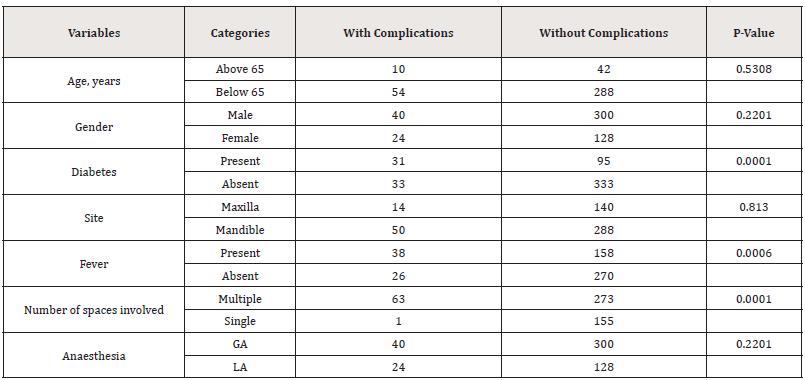
Data Management and Analysis
Data were recorded on standardized collection forms. A database was constructed using Microsoft Excel (Microsoft, Redmond, WA, USA) and imported into Epi Info version 3.5.3 for statistical analysis. Descriptive statistics were computed for all variables. Univariate analysis was carried out to see if there is any link between certain variables and life-threatening problems.
Odds ratios and p-values (based on the Chi-square test or Fisher’s exact test) were calculated. A statistically significant p-value of 0.05 was used. Significant risk factors were further analysed using multivariate logistic regression analysis.
Case Report
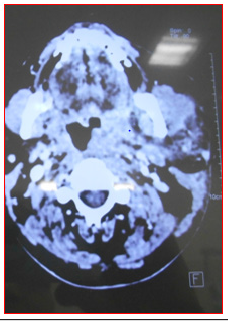
36 years old male reported to our centre referred from the peripheral centre for swelling of the face and difficulty in breathing (Figure 1,2). 48 was the offending tooth and it was removed hours back, but no decompression was carried out. The patient was given oral antibiotics without removal of the primary cause. The patient was in airway distress. There was elevation and protrusion of the tongue (Figure 3) The mouth opening was limited. He was not able to speak properly. Decompression of Submental, Sublingual and Submandibular (Figure 4,5) was done on both sides under LA. The patient was kept under follow-up. Patient was still having difficulty in breathing. So, Maxillofacial CT with Neck was done. CT scan neck (Figure 6) showed involvement of bilateral submental, sublingual, submandibular and Lt lateral pharyngeal space. In view of involvement of lateral pharyngeal space and to secure airway tracheostomy was planned for this patient. Tracheostomy was carried out for this patient. Decompression was carried out. Patient was given ICU care. Patient healed well and was discharged after closure of tracheostomy wound (Figure 7,8).
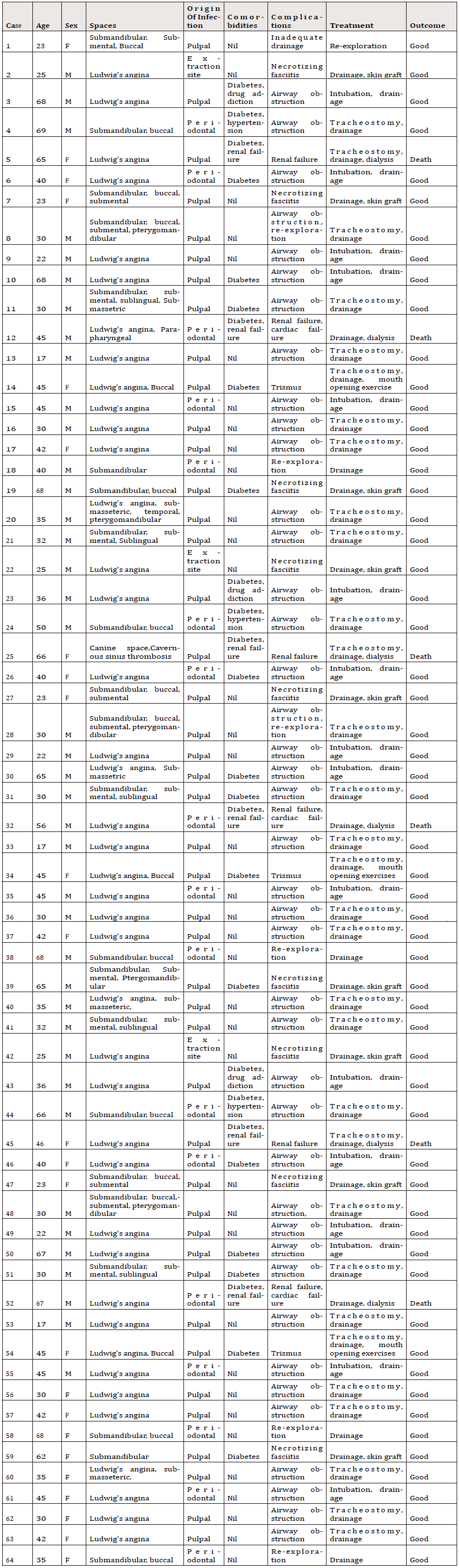
Results
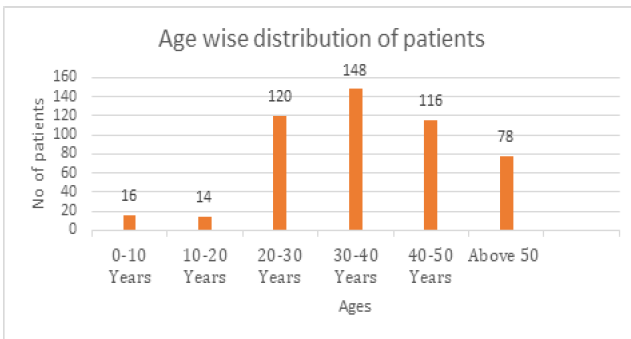
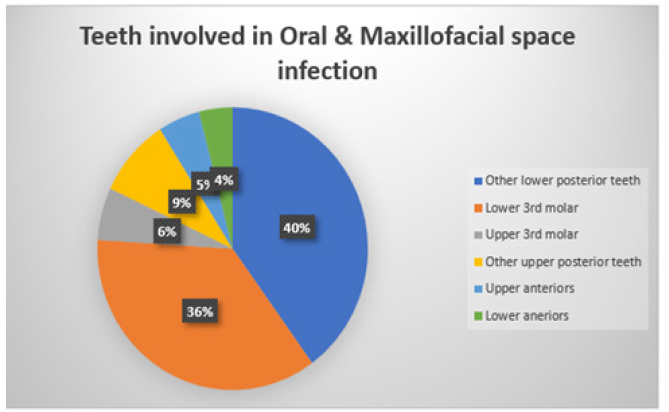
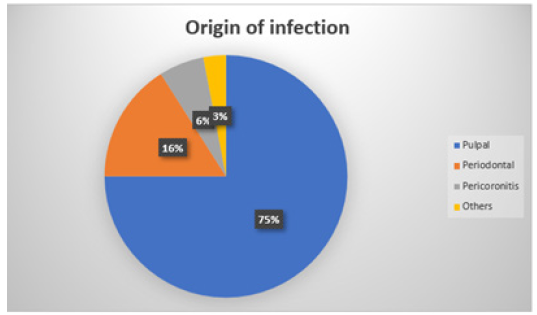
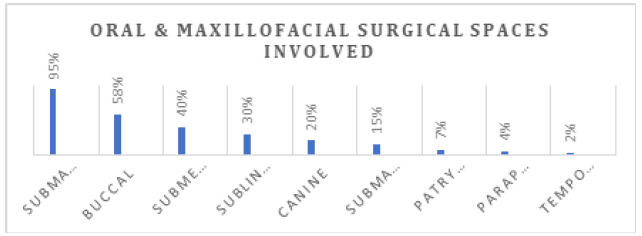
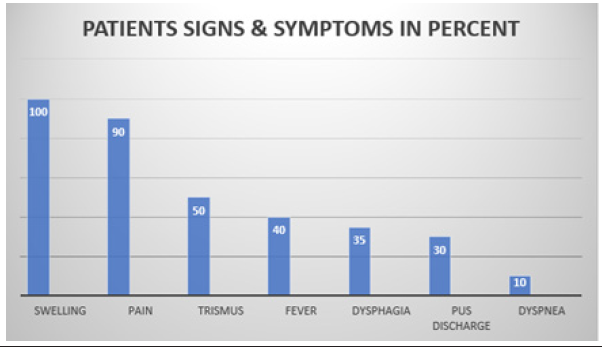
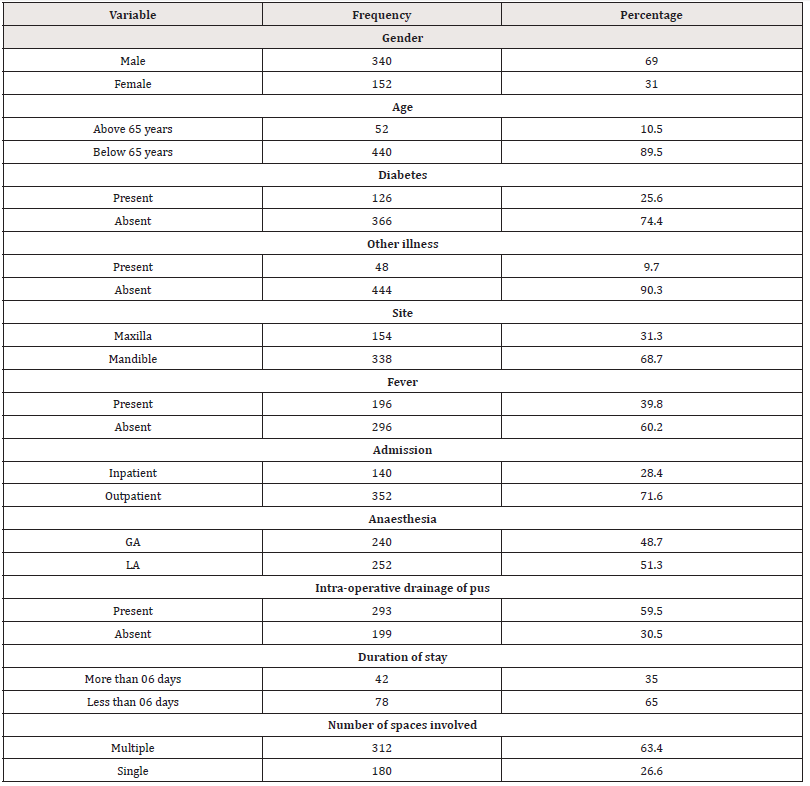
Patient characteristics - 08 patients were excluded from study because of incomplete records. Total 492 patients were included in study (Refer Table 1,2,3). The maximum patient was in the age group 30-40 (measuring 148, (Refer to Figure 9). The most commonly involved teeth were mandibular posterior teeth (Refer to Figure 10). The pattern of sign and symptoms are shown in Figure 5. Out of 492 patients, 25 % of the patients were Diabetic and 9 % of patients had other systemic illnesses like hypertension, renal disease, and CAD, etc. The origin of the infection is depicted in (Figure 11). Submandibular space was the most commonly affected space. The involvement of spaces is shown in (Figure 12,13).
26.6% patients had single space involvement; 73.7 patients had multiple space involvement. 38% patients had two spaces involved, 19% patients had three spaces involved. Rest patients were having involvement of more than three spaces Treatment – 142 patients (28.8%) were admitted for management. 350 patients (71.2%) were managed as outpatients. At the time of admission 23 patients had dyspnoea. For 8 patients’ tracheostomy was required. 390 patients were given Amoxicillin and clavulanic acid combination. Metronidazole was given for anaerobic cover. All other patients received third generation cephalosporin along with metronidazole. Amikacin or clindamycin was added in 50 patients. Surgical drainage was done under LA in 252 patients (51.3%) and under GA in 240 patients (48.7%). Out of the patient who received GA, in 160 patients (66.6%) oral intubation was done, in 72 patients (30%) nasal intubation was done. A fibreoptic intubation was done where it was indicated. In 250 patients (50.8%) extra oral incision was given. In 150 patients (30.4%) intra oral incision was sufficient for drainage. In 52 patients (10.5%), only extraction of causative teeth was sufficient for removal of infection. In 40 patients (8.1%), both extra oral and intra oral drainage was done. In 350 patients (71.1%), pus was drained during surgery. In 142 patients (28.9%) serosanguinous discharge was drained. In 440 patients (89.4%) drains were placed.
Discussion
The present study on Indian population with 492 patients and time period of 10 years is one of the few investigations on odontogenic oral & maxillofacial infection. Previously a study was done by CMC Ludhiana using 05 years of time period and 137 number of patients as parameters [9] concluded that patients with Oral & Maxillofacial space infection who present with multiple space involvement, those with diabetes and a high leukocyte count are at higher risk of developing life-threatening consequences and must be continuously watched. Odontogenic infections contribute to Oral & Maxillofacial space infection in the range of 50–89% in reports from different parts of the world. V. Yuvaraj [10] studied 2140 patients in 02 years’ time period and found that mandibular third molars were offending tooth in majority of cases, penicillin was drug used in most of cases and pterygomandibular space was most commonly involved space [11]. Ekta S Keshwani, et al in a 5-year retrospective study found maxillofacial space infection should be rendered prompt and aggressive treatment and hospitalisation should be recommended wherever required [10]. Huang, et al [12] reported 50% odontogenic infections in 185 cases of deep neck infections in Taiwan. Zhang, et al [13] reported 56.1% odontogenic infections among 212 cases of oral & maxillofacial infection in China. Bross Soriano, et al [14] reported 89% odontogenic origin infections in their 121 cases of Ludwig’s angina in Mexico. An increasing proportion of odontogenic causes among deep neck abscesses over the years has been reported by Parhiscar and Har-El from the USA [15]. These data indicate that the prevention and treatment of odontogenic infections have not been on a par with the control of other causes of Maxillofacial space infection like tonsillopharyngitis and lymphadenitis. Odontogenic infections cannot be treated only with antibiotic treatment; antibiotics are only used as a supplement to ultimate treatment. Patient’s self-medication and the primary practitioner’s failure to provide decisive therapy puts the patient at considerable danger of infection progression.
Similar to previous studies done by various investigators, the present study also confirms the finding that oral & maxillofacial infections in children are less common than adults [16,17]. The reason for more infections in adults is more population of adults as compared to children, neglect of oral hygiene and more systemic compromised adult patients. This study was conducted at a defence tertiary care centre where serving person and their dependents were treated. Person deployed at difficult duty area reported to our centre with a delay of 48 hours to 72 hours. Most of these patients were without any systemic condition. Inspite of delay, majority of these responded well to treatment and recovered without any significant complications. Most of Oral & Maxillofacial infections are odontogenic in origin. These infections occur as an outcome of a prolonged disease process. The majority of patients had recurring symptoms long before they developed a space infection. The most prevalent presenting ailment participants in our study was swelling associated with pain. Bridgeman, et al [18] observed that despite the presence of intermittent pain in the past, 98% of the patients presented for care only when there was a sudden onset of swelling. They had not sought therapy for the symptom of odontogenic pain or had received poor treatment. In our study, 50% of the patients had reached the stage of trismus, indicating that the infection had involved the masticatory spaces and could disturb the upper airway abruptly. Among these patients 10% also had dyspnoea suggesting that airway obstruction had already set in. Trismus is frequently misunderstood by dentists and patients who attribute it to other reasons. Trismus in patients with an odontogenic infection is a warning sign that necessitates a thorough evaluation for symptoms and indicator of upper airway compromise, such as tongue elevation.
In this study around 26 % of the patients were having DM. DM indicate a higher risk for Oral & Maxillofacial infections among diabetics. According to Ramachandran A et al the prevalence of diabetes among the urban population in India has been found to be 12.1% [19]. However, the percentage of diabetic patient is smaller than Huang, et al [12] stated (88.9%) [12], and Parhiscar and Har-El (50%) [15]. Immunological research has demonstrated several defects in the host immune mechanisms of diabetic subjects. Polymorphonuclear leukocytes exhibit impaired migration, phagocytosis, intracellular killing, and chemotaxis [20]. In addition to widespread immune system deficiency, several non-immunologic variables contribute to higher risk of infection. Vascular abnormalities like microangiopathy and macroangiopathy favour infection by compromising local circulation, leading to a delayed response to infection [21]. The most common origin of the Oral & Maxillofacial infections in our study was from a pulpal focus, our finding was similar to G.C. Mathew, et al [9]. The root canals are colonized by a broad mix of anaerobic bacteria once the intact pulp chamber is breached. Abscess formation occurs when these bacteria and their toxic products enter the peri-apical tissue via the apical foramen and induce acute inflammation and pus formation [22]. This pus spreads to the maxillofacial regions in close proximity to teeth’s root. This is supported by our finding that submandibular space is most commonly involved space and teeth 38 and 48 (lower wisdom teeth) are most commonly involved. Among the mandibular spaces, the submandibular space has been reported to be the most commonly involved [1,11,23,24]. The mandibular buccal [16], the lateral pharyngeal [12] and the pterygomandibular spaces [17], have been reported to be the most common in some studies. Pericoronitis leading to severe infection had a low prevalence in our study (6%), probably because pericoronitis occurs in younger individuals and is often treated immediately due to its severe symptoms. The latency in presentation to the treatment facility is the probable reason behind the higher proportion of multiple space infections compared to single space infections in our study. Other studies have also reported a preponderance of multiple space infections compared to single space infections in patients with head and neck infections of odontogenic origin [24,25].
Sato, et al [16] reported 2.85% cases with Ludwig’s angina in 210 cases of maxillofacial infections in Brazil; Uluibau, et al [26] reported 6.25% in 48 cases of severe odontogenic infection in Australia, and Huang et al, [12] reported 12.4% in a sample of 185 cases of deep neck infection in Taiwan. A 4-year prospective study at a tertiary care centre in South India [27] has reported 20 cases (18%) of Ludwig’s angina among 111 patients in a span of 4 years. We preferred tracheostomy over endotracheal intubation for airway maintenance in individuals with airway blockage. A study by Potter, et al [28] has shown that patients with deep neck infections who undergo tracheostomy for airway management spend less time in intensive care, have lower rates of complications, and when compared to patients who require endotracheal intubation, the expenditures are lower. In our study patients who had tracheostomy for airway management had an uneventful recovery. Out of all the complications, we had 41 patients presenting with Ludwig’s angina. Out of these all patients were successfully managed except 05 cases with medically compromised condition who died. Surgical drainage was performed in all patients, regardless of whether or not pus was present. The issue of cellulitis being managed differently is a carryover from a pre -antibiotic era, during which time there was a risk that surgical intervention could make the condition worse [26,29]. In every case we attribute our greater treatment success rate to our active intervention. The only 07 deaths that occurred in the study sample were of patients with diabetes and chronic renal failure, where the systemic condition led to death. Out of these 01-patient developed cavernous sinus thrombosis as complication and 06 patients developed Ludwig angina. Currently there is an evolving consensus that the difference between cellulitis and abscess is no longer clinically relevant and that both need to be drained [26].
In our study, we did not perform pus culture as in India there is a high rate of self-prescription and over-the-counter medication among patients. Patients with oral infections see a variety of dentist and seek symptomatic alleviation rather than receiving thorough treatment. Most patients have been on several courses of antibiotics before they present to a tertiary centre with a severe infection [30]. The bacteriology of severe odontogenic infections, though subtly different from that of the acute dental abscess, is still a complex mixture of strict anaerobes and facultative anaerobes, the culture of which can prove challenging for a non-specialist microbiology laboratory [22-30]. All our patients had a good response to the antibiotics and metronidazole, as well as surgical drainage. Betalactam antibiotics have long been used to treat odontogenic infections because they are highly efficient against the bacteria that cause them, are inexpensive, and have little side effects. The increasing rate of beta-lactam resistance due to the emergence of beta-lactamase-producing organisms has led to concerns regarding the effectiveness of eta-lactam antibiotics [31]. There hasn’t any agreement on a standard antibiotic protocol, owing to a lack of data in the form of well-designed clinical trials to support one regimen over another [32]. We have treated all patients with serious Oral & Maxillofacial surgery with a standard regimen of beta-lactamase stable beta-lactam antibiotic and metronidazole, as in these patients with impending airway obstruction, any delay in instituting an effective treatment can lead to death, and the local rates of beta-lactam resistance are very high. The combination of these antibiotics provides an antibiotic spectrum against the viridans streptococci and the strict anaerobes that are predominant in odontogenic infections [30]. Few studies have looked at patient characteristics associated with complications in Oral & Maxillofacial surgery. Diabetes [13,24] and multiple space involvement [24] have already been noted to be significantly associated with lifethreatening complications. We have identified that patients with diabetes, multiple space involvement, or a total leukocyte count more than 15000 per cubic mm on admission tend to develop complications during treatment. Other studies have also noted that well-managed diabetes can lead to a prognosis similar to that of a non-diabetic with similar severity of infection [27,33]. Good control of blood sugars and aggressive management of the diabetic patient with multiple space infection and a high leukocyte count can ensure a reduction in complications during the course of treatment.
Acknowledgement
Our acknowledge to each person who has helped in any manner in successful completion of this study.
Conflict of Interest
No conflict of interest.
References
- Kuo J, Lin Y, Lin YT (2013) Odontogenic cellulitis in children requiring hospitalization. J Dent Sc 8: 129-132.
- Reynolds SC, Chow AW (2007) Life-threatening infections of the peripharyngeal and deep fascial spaces of the head and neck. Infect Dis Clin North Am 21: 557-576.
- Kao S, Jo C (2014) Oral and Maxillofacial Infections. Clinical review of oral and maxillofacial surgery: 95-118.
- Barsamian JG, Scheffer RB (1987) Spontaneous pneumothorax: an unusual occurrence in a patient with Ludwig’s angina. J Oral Maxillofac Surg 45: 161-168.
- Wong TY (1999) A nationwide survey of deaths from oral and maxillofacial infections: the Taiwanese experience. J Oral Maxillofac Surg 57: 1297-1299.
- Colmenero RC, Labajo AD, Yanez Vilas I, Paniagua J (1993) Thoracic complications of deeply situated serous neck infections. Craniomaxillofacial Surg 21(2): 76-81.
- Roberson JB, Harper JL, Jauch EC (1996) Mortality associated with cervicofacial necrotizing fasciitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 82: 264-267.
- Umeda M, Minamikawa T, Komatsubara H, Shibuya Y, Yokoo S, et al. (2003) Necrotizing fasciitis caused by dental infection: a retrospective analysis of 9 cases and a review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 95(3): 283-290.
- GC Mathew, Laxman Kumar Ranganathan, Sumir Gandhi, Mini Elizabeth Jacob, Inderjot Singh, et al. (2012) Odontogenic maxillofacial space infections at a tertiary care center in North India: a five-year retrospective study. Int J Infect Dis 16(4): e296-e302.
- V Yuvaraj (2016) Maxillofacial Infections of Odontogenic Origin: Epidemiological, Microbiological and Therapeutic Factors in an Indian Population. Indian J Otolaryngol Head Neck Surg 68(4): 396-399.
- Ekta S Keswani, Gokul Venkateshwar (2019) Odontogenic Maxillofacial Space Infections: A 5-Year Retrospective Review in Navi Mumbai. J Maxillofac Oral Surg 18(3): 345-353.
- Huang TT, Liu TC, Chen PR, Tseng FY, Yeh TH, et al. (2004) Deep neck infection: analysis of 185 cases. Head Neck 26(10): 854-860.
- Zhang C, Tang Y, Zheng M, Yang J, Zhu G, et al. (2010) Maxillofacial space infection experience in West China: a retrospective study of 212 cases. Int J Infect Dis 14(5): e414-417.
- Bross Soriano D, Arrieta Gomez JR, Prado Calleros H, Schimelmitz Idi J, Jorba Basave S, et al. (2004) Management of Ludwig’s angina with small neck incisions: 18 years’ experience. Otolaryngol Head Neck Surg 130(6): 712-717.
- Parhiscar A, Har El G (2001) Deep neck abscess: a retrospective review of 210 cases. Ann Otol Rhinol Laryngol 110(11): 1051-1054.
- Sato FR, Hajala FA, Filho FW, Moreira RW, Márcio de Moraes, et al. (2009) Eight-year retrospective study of odontogenic origin infections in a postgraduation program on oral and maxillofacial surgery. J Oral Maxillofac Surg 67(5): 1092-1097.
- Flynn TR, Shanti RM, Levi MH, Adamo AK, Kraut RA, et al. (2006) Severe odontogenic infections, part 1: prospective report. J Oral Maxillofac Surg 64: 1093-1103.
- Bridgeman A, Wiesenfeld D, Hellyar A, Sheldon W (1995) Major maxillofacial infections. An evaluation of 107 cases. Aust Dent J 40(5): 281-288.
- Ramachandran A, Snehalatha C, Kapur A, Vijay V, Mohan V, et al. (2001) High prevalence of diabetes and impaired glucose tolerance in India: National Urban Diabetes Survey. Diabetologia 44(9): 1094-1101.
- Valerius NH, Eff C, Hansen NE, Karle H, Nerup J, et al. (1982) Neutrophil and lymphocyte function in patients with diabetes mellitus. Acta Med Scand 211: 463-467.
- Goodson III WH, Hunt TK (1979) Wound healing and the diabetic patient. Surg Gynecol Obstet 149(4): 600-608.
- Robertson D, Smith AJ (2009) The microbiology of the acute dental abscess. J Med Microbiol 58(2): 155-162.
- Rega AJ, Aziz SR, Ziccardi VB (2006) Microbiology and antibiotic sensitivities of head and neck space infections of odontogenic origin. J Oral Maxillofac Surg 64(9): 1377-1380.
- Boscolo Rizzo P, Da Mosto MC (2009) Submandibular space infection: a potentially lethal infection. Int J Infect Dis 13(3): 327-333.
- Storoe W, Haug RH, Lillich TT (2001) The changing face of odontogenic infections. J Oral Maxillofac Surg 59(7): 739-748.
- Uluibau IC, Jaunay T, Goss AN (2005) Severe odontogenic infections. Aust Dent J 50(4 Suppl 2): S74-81.
- Rao DD, Desai A, Kulkarni RD, Gopalkrishnan R, Rao CB, et al. (2010) Comparison of maxillofacial space infection in diabetic and non diabetic patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 110(4): e7-12.
- Potter JK, Herford AS, Ellis E (2002) Tracheostomy versus endotracheal intubation for airway management in deep neck space infections. J Oral Maxillofac Surg 60(4): 349-354.
- Goldberg MH, Topazian RG (2002) Odontogenic infections and deep fascial space infections of dental origin. Oral and maxillofacial infections 4th edn: 198-250.
- Kotwani A, Holloway K (2011) Trends in antibiotic use among outpatients in New Delhi, India. BMC Infect Dis 11: 99.
- Kuriyama T, Karasawa T, Nakagawa K, Saiki Y, Yamamoto E, et al. (2000) Bacteriologic features and antimicrobial susceptibility in isolates from orofacial odontogenic infections. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 90(5): 600-608.
- Robertson D, Smith AJ (2009) The microbiology of the acute dental abscess. J Med Microbiol 58: 155-162
- Peralta G, Sa´nchez MB, Roiz MP, Garrido JC, Teira R, et al. (2009) Diabetes does not affect outcome in patients with Enterobacteriaceae bacteremia. BMC Infect Dis 9: 94.









 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.